Introduction
The ‘Can’t Intubate Can’t Oxygenate’ (CICO) situation is a life-threatening, time-critical airway emergency.1 Although a rare event, it is associated with significant patient morbidity and mortality.1 The 4th National Audit Project by the Royal College of Anaesthetists (RCOA) and Difficult Airway Society (DAS) highlighted multiple factors influencing CICO outcome.2 A major modifiable factor included the availability and accessibility of essential equipment.2 The purported ergonomic utility of pre-packaged CICO equipment into kits has also been recently described in literature.3 However, there remains a lack of evidence in current literature to support the superiority of any one packaged design or inferences as to its impact on task performance.
At Fiona Stanley Hospital, the Vortex approach and Vortex CICO status tool are used for in-theatre emergency airway and CICO crisis management, respectively. As part of the Vortex CICO status tool, there exists a recommendation for the use of a CICO ‘kit’ as part of its staged ‘ready, set, go’ response.4 The Australian and New Zealand College of Anaesthetists (ANZCA) also advocates in its professional documents (Policy Statement 61) that the choice of equipment be matched to guidelines and cognitive aids in order to avoid ambiguity and minimise delays in a crisis.5 This facilitates the timely transition from failed supraglottic airway (SGA) attempts down towards infraglottic airway rescue.
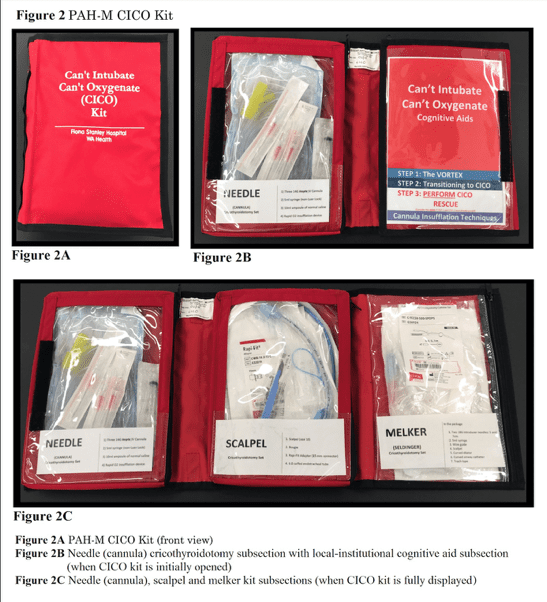
Whilst the choice of infraglottic rescue technique remains contentious, Greenland et al aptly point to the fact that anaesthetists should be capably trained in more than one infraglottic airway rescue technique.6 In this context, the repertoire of skills should be equally matched by the availability of CICO equipment. A comprehensive, pre-packaged CICO kit that presents all available infraglottic rescue options has been developed by Foong et al and is currently in use at Princess Alexandra Hospital (Brisbane, Queensland).3 A modified version of this kit (PAH-M) was developed to compare against institutionally packaged CICO equipment (FSH kit).7 Local-institutional algorithms and cognitive aid resources complemented the CICO kit.
Physiological stress is an important factor that can augment or hinder task performance during a crisis.8 Environmental factors in the operating theatre such as noise, lighting, location and equipment may contribute to the stress load. More specifically, the layout, design, presentation and utility of a CICO kit may impact the stress experienced by clinicians managing a CICO crisis.
The primary objective of this pilot study was to investigate the impact of the CICO kits and their ergonomics on the timed responses of participants in a simulated CICO crisis. A secondary objective was to assess whether a difference in physiological stress exists between CICO kit groups.
Methods
The study was registered with the Australian and New Zealand Clinical Trials Registry (ACTRN 126190 00001190) prior to participant enrolment. A total of 12 paired participants consisting of an anaesthetic provider (e.g. consultant or registrar) and anaesthetic technician were recruited (n = 24) from the Department of Anaesthesia, Pain and Perioperative Medicine at Fiona Stanley Hospital. Paired participants were initially randomised for testing by coin toss, to either the PAH-M kit or FSH kit, using a simulated CICO crisis as described below. The simulation was repeated using the other kit. This crossover study design allows assessment of possible order of effects by within-pairs comparison.
At Fiona Stanley Hospital, CICO equipment is organised and stored separately on both the airway trolley and difficult airway trolley. Attached to the airway trolley is a transparent sleeve containing preliminary essential equipment, which contains a size 10 scalpel, Rapi-fit adaptor, size 6 endotracheal tube, and, two items each of the following: 14-gauge Insyte cannula, 5ml syringe and 20mls of normal saline. The sleeve is positioned adjacent to a Rapid O2 device and bougie (Cook ® Frova Intubating Introducer). Additional needle crico-thyroidotomy equipment is available within the airway trolley drawers. A ‘Universal Melker kit’ is available within the difficult airway trolley, which must be separately retrieved (Fig. 1). A self-inflating bag is located behind the mechanical ventilator. This ad hoc combination of equipment is referred to as the FSH kit.

By comparison, the PAH-M kit can be considered as a comprehensive folder containing all essential CICO equipment (Fig. 2). The design of the folder by Foong et al reveals three compartments for equipment (cannula, scalpel-bougie and Melker (Seldinger) cricothyroidotomy subsections) and a fourth compartment for local-institutional cognitive aids and resources.3 The displayed sequence of equipment subsections, local institutional algorithms used and both choice and number of equipment pieces available align with our institutional training, which is based on the Royal Perth Hospital CICO algorithm by Heard et al.9
The clinical simulation was of a 35-year-old male planned for an emergency laparotomy on the background of an acutely perforated small bowel obstruction. Documented airway assessment included Mallampati grade 4, a shortened thyromental distance, reduced mouth opening and limited neck extension. Participants were instructed to plan and prepare for a general anaesthetic.
The simulation was conducted in an operating theatre. Pre-induction SIM-man 3G settings included a blood pressure of 130/80 mmHg, sinus tachycardia of 130 beats/minute and pulse oximetry (SpO2) reading of 98%. On successive failed attempts at supraglottic airway management, SpO2 values were gradually decreased from 98% to 82% with a concomitant rising tachycardia. The crisis evolved over a period of 90 seconds from the start of the simulation. Successful cricothyroidotomy resulted in an initial 5% rise in SpO2. To avoid inadvertently distracting participants into preparing for a possible cardiac arrest, the minimum permitted pulse oximeter reading was 82%.
A separate impalpable front of neck mannequin was provided for when infraglottic rescue was to be performed. Participants were instructed to conduct themselves in their usual occupational capacity. A debrief session was conducted after each simulation with a short washout period of less than 30 minutes between simulations.
Pre- and post-simulation questionnaires were conducted. These included questions related to socio-demographic, occupational and physiological stress parameters. The latter involved physiological stress variables related to quality of sleep, caffeine intake, hunger, emotion, cognitive stress, and arousal state. Electronic heart monitoring devices were worn by the study participants.
Statistical analyses were conducted by the Centre for Applied Statistics, Department of Mathematics and Statistics at the University of Western Australia. T-tests were used to assess for differences in means and a linear regression model used to adjust for a carry-over learning effect.
Results
Randomisation of paired participants (12 paired groups) was performed to allocate groups to an initial CICO kit (PAH-M kit, 7 paired groups vs FSH kit 5 paired groups) with a subsequent crossover design. The paired groups consisted of anaesthetic consultants (2), senior (8) or junior (2) anaesthetic registrars and anaesthetic assistants (n = 12).
In the PAH-M kit group, 8 of the 12 paired participants chose a cannula technique, whilst the remaining 4 pairs chose a scalpel technique. In the FSH kit group, 6 of the 12 paired participants chose a cannula technique and the remaining 6 pairs chose a scalpel technique. In the FSH kit group, one pair who initially chose a cannula technique subsequently failed and converted to a scalpel technique.
A comparison of primary timed outcomes for the CICO kit groups is shown in Table 1. The rationale for having two different commencement times in relation to the primary outcomes will be discussed later. Whilst the difficult airway trolley was present within the operating theatre, the time to ‘ventilation + time constant’ outcome describes a potential situation in which the difficult airway trolley had to be separately retrieved by the anaesthetic technician in the FSH kit group.

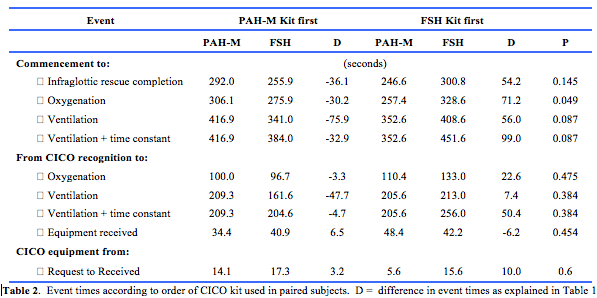
An order of effects model was used to compare mean time differences between CICO kit groups depending on which kit was performed first (Table 2). The order of effects analysis from timed commencement of simulation to oxygenation demonstrated a statistically significantly faster time for the CICO kit (p=0.049).
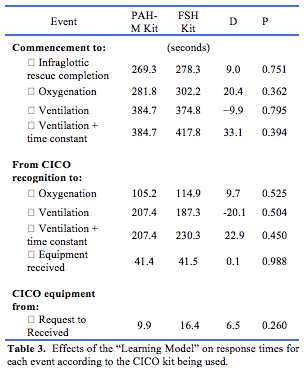
Linear regression was used to adjust for the carry-over learning effects due to repetition of the CICO simulation. As a result, the learning model shows the average times without the learning effect (Table 3), which allows for an assessment of any time difference using the PAH-M kit as the point of reference. Whilst no one timed outcome achieved statistical significance, the fact that the PAH-M kit always has a time advantage especially after adjustment of ventilation by a time constant and across seven measures is indicative of its effectiveness. The difference in baseline heart rate to maximal heart rate was calculated for each participant. A comparison of the mean heart rate differences between CICO kit groups did not reach statistical significance (PAH-M vs. FSH mean difference 1.2 beats/minute (SD 10.2 beats/minute, p = 0.564).
The results of questionnaires reporting participant perceptions of stress and the perceived impact of stress on performance are tabulated separately in appendices 1 and 2, respectively.
Discussion
In comparison to our institutional kit, the PAH-M kit demonstrates an overall time advantage across discrete timed events. Of particular clinical relevance is time to oxygenation. A poorly managed CICO event can lead to irreversible hypoxic brain injury and this may occur within several minutes followed by cardiovascular collapse.10 In this context, differences in the order of seconds are clinically meaningful as it can mean the difference between life and death.
The order of effects model in favour of the PAH-M kit for time to oxygenation may be due to its ergonomic design. A possible explanation is that the PAH-M kit confers a higher degree of ergonomic utility and user-friendliness within a crisis situation. It is also complemented by clear labelling of equipment subsections and local-institutional cognitive aids. A study by Marshall and Mehra found that the use of cognitive aids led to higher ANTS (Anaesthetists’ Non-Technical Skills) scores for infra-glottic airway rescue.11 Furthermore, the primary outcomes studied can be distinguished according to their recorded starting times. For example, the primary objectives were measured either from the start of the simulation or from a predetermined time point such as participant recognition of a CICO event. The former captures the full breadth of the CICO crisis event, which is affected by anaesthetic management, crisis resource management, human- and procedural-related factors. The latter time period focuses on the CICO transition phase and performance of infraglottic rescue. From a simulation and crisis response perspective, this distinction helps one to appreciate the multiple factors influencing CICO rescue outcomes.
Unique to this pilot study is the use of high fidelity, immersive simulations to assess timed outcomes related to a critically important aspect of airway crisis management. It allows for the complex interplay between the anaesthetist and their assistant to fully evolve as would normally occur in clinical practice. The successful management of the simulated crisis is thus dependent on the effective use of both technical and non-technical skills.
Whilst proponents may argue the superiority of one infraglottic rescue technique over another and prescribe its use in CICO management,12,13 this study instead gave participants the autonomy to select their own preferred technique. This serves to replicate the actual dynamic responses participants would display when challenged by an actual airway crisis. The focus is thus shifted to the achievement of the primary objectives of this pilot study rather than the particular front of neck access technique used.
Whilst the self-reported impact of stress on performance between CICO kit groups for initial and subsequent CICO simulations overall appear to trend lower for the PAH-M kit, heart rate variability comparisons did not demonstrate statistical significance. It is possible that participants immersed in sequential high intensity crisis simulations may not have had enough time to demonstrate the physiological changes due to a short washout time period. We recommend that an extended washout time period be considered in future research.
ConclusionThe ergonomic utility of a CICO kit has an influence on time-critical outcomes in simulated CICO crises and ongoing research is highly recommended. Surrogate measures of the impact of stress on procedural performance such as heart rate monitoring remains an interesting area for future research.
Provenance: Externally reviewed
Ethics Approval: South Metropolitan Health Service Human Research Ethics committee.
Conflicts of Interest: Nil
Funding: CICO kit folder was supplied by Queensland Case Medikit, 3/13 Veronica Street Capalaba QLD 4157 and Melker Seldinger kit was supplied by Cook Medical.
Acknowledgements: We thank Dr Wai Mee Foong, Anaesthetic Department, Princess Alexandra Hospital, Brisbane, Queensland Australia for commenting on the manuscript.
Corresponding Author: Dr Justin Shih Sunn Ti, Department of Pain and Perioperative Medicine, Fiona Stanley Fremantle Hospitals Group, Murdoch, WA 6150, Australia. Email: justin.ti@health.wa.gov.au











